Research overview: MAMMOGRAPHIC DENSITY, PHYSICAL ACTIVITY AND BREAST CANCER
Written by: Dr. Noelle Cutter / Sept. 12, 2021
Edited by: the publishing team @ NYCRANEWS.com
Mammography, as the primary screening modality, has facilitated a substantial decrease in breast cancer-related mortality in the general population. However, the sensitivity of mammography for breast cancer detection is decreased in women with higher breast densities, which is an independent risk factor for breast cancer. With increasing public awareness of the implications of a high breast density, there is an increasing demand for supplemental screening in these patients. Yet, improvements in breast cancer detection with supplemental screening methods come at the expense of increased false-positives, recall rates, patient anxiety, and costs. Therefore, breast cancer screening practice must change from a general one-size-fits-all approach to a more personalized, risk-based one that is tailored to the individual woman's risk, personal beliefs, and preferences, while accounting for cost, potential harm, and benefits.
FACTOIDS & FIGURES- The Inspiration behind our research initiative [1]:
▪ Breast cancer is the second most common cancer among women in the United States and about 1 in 8 U.S. women (about 13%) will develop invasive breast cancer over the course of her lifetime.
▪ In 2021, it is estimated that over 280,000 new cases of invasive breast cancer will be diagnosed in women in the U.S.,
▪ Over 40,000 women in the U.S. are expected to die in 2021 from breast cancer. Unfortunately, death rates have been steady in women under 50 since 2007, despite advancements in treatment options.
▪ For women in the U.S., breast cancer death rates are higher than those for any other cancer, besides lung cancer.
▪ As of January 2021, there are more than 3.8 million women with a history of breast cancer in the U.S. This includes women currently being treated and women who have finished treatment.
▪ Breast cancer is the most commonly diagnosed cancer among American women. In 2021, it's estimated that about 30% of newly diagnosed cancers in women will be breast cancers.
▪ Breast cancer became the most common cancer globally as of 2021, accounting for 12% of all new annual cancer cases worldwide, according to the World Health Organization.
▪ A woman’s risk of breast cancer nearly doubles if she has a first-degree relative (mother, sister, daughter) who has been diagnosed with breast cancer.
 |
| Click for full lecture with Dr. N. Cutter & Dr. L. Bard |
▪ About 85% of breast cancers occur in women who have no family history of breast cancer.
The most significant risk factors for breast cancer are sex (being a woman) and age. But recent research is beginning to clarify additional risk factors associate with BC
PHYSICAL ACTIVITY
Physical activity is considered a significant modifiable factor in breast cancer risk, and since exercise reduces fatty tissue and BMI, it has been thought to increase breast density. However, studies into the relationship between physical activity and breast density have been inconclusive. Other factors such as alteration in metabolism of endogenous hormones, are suggested to influence mammographic density (MD) as well. Therefore, it is evident that the links between physical activity and breast cancer risk need to be clarified.
BREAST TISSUE DENSITY
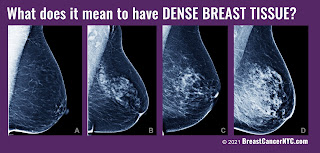
Breast density levels refer to the appearance of the breast tissue on a mammogram. Breast density is part of the supportive or connective tissue that makes up the breast tissue. As you can see in this image, breast tissue is white to gray and transparent against a dark background. Denser breast tissue appears more white whereas fatty/non-dense tissue appears grapy and transparent.
Levels of density are described using a results reporting system called Breast Imaging Reporting and Data System (BI-RADS). The levels of density are often recorded in your mammogram report using letters. The levels of density are:
A: Almost entirely fatty indicates that the breasts are almost entirely composed of fat. About 1 in 10 women has this result.
B: Scattered areas of fibroglandular density indicates there are some scattered areas of density, but the majority of the breast tissue is non-dense. About 4 in 10 women have this result.
C: Heterogeneously dense indicates that there are some areas of non-dense tissue, but that the majority of the breast tissue is dense. About 4 in 10 women have this result.
D: Extremely dense indicates that nearly all of the breast tissue is dense. About 1 in 10 women has this result.
In general, women with breasts that are classified as heterogeneously dense or extremely dense are considered to have dense breasts. Almost half of women undergoing mammograms have dense breasts.
A close up here shows the difference in imaging for a breast tumor on non-dense vs dense breast tissue using a mammogram. Breast density has been widely considered a strong risk factor for breast cancer, with statistics suggesting as much as a six times higher likelihood of the disease in breasts, compared with those with a less dense breast tissue. Not only does dense breast tissue make it harder for a mammogram to pick up small tumors, but dense breasts themselves have been associated with a higher chance of cellular abnormality.
WHY IT MATTERS?
Women who have dense breast tissue have a higher risk of breast cancer compared to women with less dense breast tissue. It’s unclear at this time why dense breast tissue is linked to a higher lifetime risk of breast cancer. Understanding that link is extremely important.
Dense breast tissue also makes it harder for radiologists to see cancer. On mammograms, dense breast tissue looks white. Breast masses or tumors also look white, so the dense tissue can hide tumors. But fatty tissue looks almost black. On a black background it’s easier to see a tumor that looks white. So, mammograms can be less accurate in women with dense breasts.
One of the challenges in promoting the widespread utility of breast cancer risk prediction models has been the assertion that most women with a diagnosis of breast cancer have no established clinical breast cancer risk factors or are not considered to be high risk. [1][2] Although it is impossible to determine the cause of breast cancer in any individual case [3] easily assessed risk factors that explain a substantial proportion of incident breast cancers can be used to stratify breast cancer risk for targeted screening [4] and primary prevention [5] and improve public health interventions to reduce breast cancer risk.
Recent research has suggested that for women with dense breasts, a screening strategy that also takes into account a woman’s risk factors and protective factors may be the best predictor of whether a woman will develop breast cancer after a normal mammogram and before her next scheduled mammogram.
MAMMOGRAPHIC DENSITY
Breasts contain glandular, connective, and fat tissue. Breast density is a term that describes the relative amount of these different types of breast tissue as seen on a mammogram. Dense breasts have relatively high amounts of glandular tissue and fibrous connective tissue and relatively low amounts of fatty breast tissue.
HOW COMMON ARE DENSE BREASTS?
Nearly half of all women age 40 and older who get mammograms are found to have dense breasts. Breast density is often inherited, but other factors can influence it. Factors associated with lower breast density include increasing age, having children, and using tamoxifen. Factors associated with higher breast density include using postmenopausal hormone replacement therapy and having a low body mass index.
Women with dense breasts have a higher risk of breast cancer than women with fatty breasts, and the risk increases with increasing breast density. This increased risk is separate from the effect of dense breasts on the ability to read a mammogram. MD one of the strongest risk factors. And because individuals with denser breasts tend to develop more serious types of breast cancer, understanding the connection is important.
ATHLETES
A common question that invariably comes up when discussing breast density relates to breast density in athletes. As an athlete myself who has dense breasts, I was struck by the number of individuals in my athletic community who also have dense breasts. A shocking trend was seen in the overwhelming amount of young women with dense breasts who subsequently had received false negative mammogram reports.
What we do know is that your breast tissue tends to become less dense as you age, though some women may have dense breast tissue at any age. Women with less body fat are more likely to have more dense breast tissue compared with women who are obese. From observation (thus far), athletic women are also more likely to have dense breast tissue. One of the main goals of our study is to really try to understand the biological connection of breast density in athletes as well as run a retrospective study on how common this trend is.
RESEARCH OBJECTIVES
It's not clear why some women have a lot of dense breast tissue and others do not. You may be more likely to have dense breasts if you:
▪ ARE YOUNGER; your breast tissue tends to become less dense as you age, though some women may have dense breast tissue at any age.
▪ HAVE LOWER BMI (body mass index); women with less body fat are more likely to have more dense breast tissue compared with women who are obese.
Breast density is shown to be associated with breast cancer risk in women aged 40 to 65 years, but there is limited evidence thus far of its association with risk of breast cancer among women 18+. Furthermore, a high proportion of women with low BMI present with dense breasts, making them likely candidates to receive false negative readings on a mammogram. We aimed to estimate the proportion of breast cancers attributable to breast cancer risk factors commonly documented in clinical practice and used in breast cancer risk prediction models, including BI-RADS breast density and ultrasounds to confirm mammography readings. Our data will be collected from a cohort of women undergoing ultrasound density scans at the Bard Cancer Center (NYC).Although breast density is a well-established, strong, and prevalent breast cancer risk factor it’s biological connection is not clearly understood. More research is needed to support the population associated risk proportion in athletic pre-menoposal women. Our data will start with a cohort of women undergoing imaging ultrasounds at the Bard Cancer Diagnostic Center. Our population will include pre-menoposal women with dense breasts.
METHODS
Endurance athletes are defined those who participated in one or more endurance events (long course) in the year or as well as those who are (younger, low BMI cohort). MD and classification of “dense breasts” was heterogeneous and extremely dense as noted by the BI_RADS code; (heterogeneously or extremely dense vs scattered fibroglandular densities). Data will be collected as odds ratio (OR’s) and 95% confidence intervals included in our outcomes
Cross-sectional Analysis |
1000+ pre-menopausal women aged 18+ |
Collect information on height, weight, BMI and history of disease |
Physical activity assessment |
MD measurement performed by radiologist and confirmed by ultrasound |
Logistic regression used to estimate the association of MD within participation in physical activity |
JAMA STUDY:
A recent report in Journal of the American Medical Association found that first-degree family history of breast cancer dense breasts were associated with an increased population associated risk proportion of breast cancer. Among premenopausal women, the largest individual population associated risk proportion was for breast density, with 28.9% (95% CI, 25.3%-32.5%) of breast cancers potentially removed by reducing breast density from BI-RADS heterogeneously or extremely dense breasts to scattered fibroglandular densities. The population associated risk proportion for breast density increased to 65.5% (95% CI, 60.4%-70.6%) if all premenopausal women reduced their breast density to the lowest category of almost entirely fat tissue.
SUMMARY/ WRAP-UP
Given that greater breast density as categorized by the BI-RADS remains a factor associated with breast cancer for all ages of women, information about breast density together with life expectancy may benefit clinical decision-making regarding screening. In March 2019, the US Food and Drug Administration recommended changes to the Mammography Quality Standards Act to make it mandatory to report breast density information to both patients and their physicians. However, how women and their physicians should use this information to inform screening recommendations is unclear. Very dense breasts may increase the risk that cancer won't be detected on a mammogram.
What is clear is that additional research is needed to elucidate the mechanisms underlying the observed associations between breast density and risk of breast cancer. As newer and more advanced breast density assessment techniques are developed, evaluation of the diffusion of such innovations with an aim of developing individualized screening strategies will be important, particularly among athletic women, for whom dense breast are more likely seen.
EPILOGUE
Dr. Noelle Cutter is a professor of biology, ironman finisher, and advocate for dense breast screening. United with an expanding research team dedicated to collecting data on women with dense breasts and screening options for these patients, her initiative aims to investigate and gather conclusive information about dense breasts in specific groups- including age, body mass index, and amount of physical activity and the underlying diagnostics of breast cancer tumors. This research program is under a partnership with Molloy College and Dr. Robert Bard, expert diagnostic cancer imaging specialist in NYC and other colleagues from the NY Cancer Resource Alliance.With your support, we are able to implement this screening program for women's health as well as help fund this clinical research. Our work will advance technology, change legislation and most importantly save lives through awareness.
On July 27-29, Bard Diagnostic Imaging is offering a comprehensive DENSE BREAST SCREENING DAY, employing an array of imaging advancements dedicated to the visibility of dense breast tissue and cancer early detection. This special program is dedicated to supporting dense breasted patients by first identifying one's actual breast density (through a density assessment scan) to establish a base line for the full diagnostic study (est. 15-20 minutes per patient).
Dr. Bard has formulated a comprehensive early detection program specific for dense breasted women. This includes the latest technologies in breast ultrasound, scanning. "We need screening technology for dense breasts because the mammography misses too many cancers in dense breast. So patients are happy to know that this technology is here. If there is a problem, you focus in on it in three dimensions, you find out where it is, and then you, uh, address it with a biopsy or an MRI or a specialized ultrasound." For decades. The ultrasound has advanced greatly in accuracy and reliability to scan quickly. In real time, patients are attracted to its safety aspect, eliminating concerns for radiation and other physical after effects.
REFERENCES
1) https://www.breastcancer.org/symptoms/understand_bc/statistics
2) Cruwys, Cheryl, and JoAnn Pushkin. “Breast density and impacts on health.” ecancermedicalscience 11 (2017).
3) Nazari, Shayan Shaghayeq, and Pinku Mukherjee. “An overview of mammographic density and its association with breast cancer.” Breast cancer 25.3 (2018): 259-267.
4) Boyd, Norman F., et al. “Mammographic density: a heritable risk factor for breast cancer.” Cancer epidemiology. Humana Press, 2009. 343-360.
5) Burton, Anya, et al. “Mammographic density and ageing: A collaborative pooled analysis of cross-sectional data from 22 countries worldwide.” PLoS medicine 14.6 (2017): e1002335.
6) Azam, Shadi, et al. “Determinants of mammographic density change.” JNCI Cancer Spectrum 3.1 (2019): pkz004.
7) Boyd, Norman F., et al. “Body size, mammographic density, and breast cancer risk.” Cancer Epidemiology and Prevention Biomarkers 15.11 (2006): 2086-2092.
8) Masala, Giovanna, et al. “Can Dietary and Physical Activity Modifications Reduce Breast Density in Postmenopausal Women? The DAMA Study, a Randomized Intervention Trial in Italy.” Cancer Epidemiology and Prevention Biomarkers 28.1 (2019): 41-50.
9) Wyshak, Grace, and Rose E. Frisch. “Breast cancer among former college athletes compared to non-athletes: a 15-year follow-up.” British journal of cancer 82.3 (2000): 726.
10) McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15(6):1159-1169.
Disclaimer & Copyright Notice: The materials provided on this website/web-based article are copyrighted 2021 and the intellectual property of the publishers/producers (The NY Cancer Resource Alliance/IntermediaWorx inc. and Bard Diagnostic Research & Educational Programs). It is provided publicly strictly for informational purposes within non-commercial use and not for purposes of resale, distribution, public display or performance. Unless otherwise indicated on this web based page, sharing, re-posting, re-publishing of this work is strictly prohibited without due permission from the publishers. Also, certain content may be licensed from third-parties. The licenses for some of this Content may contain additional terms. When such Content licenses contain additional terms, we will make these terms available to you on those pages (which his incorporated herein by reference).The publishers/producers of this site and its contents such as videos, graphics, text, and other materials published are not intended to be a substitute for professional medical advice, diagnosis, or treatment. For any questions you may have regarding a medical condition, please always seek the advice of your physician or a qualified health provider. Do not postpone or disregard any professional medical advice over something you may have seen or read on this website. If you think you may have a medical emergency, call your doctor or 9-1-1 immediately. This website does not support, endorse or recommend any specific products, tests, physicians, procedures, treatment opinions or other information that may be mentioned on this site. Referencing any content or information seen or published in this website or shared by other visitors of this website is solely at your own risk. The publishers/producers of this Internet web site reserves the right, at its sole discretion, to modify, disable access to, or discontinue, temporarily or permanently, all or any part of this Internet web site or any information contained thereon without liability or notice to you.