By: Robert L. Bard, MD & Noelle Cutter, PhD | Edited by: Lennard M. Gettz, Ed.D
PROLOGUE
In 2014, Imaging Technology News (ITN) introduced breast cancer survivor-turned-crusader Dr. Nancy Cappello and her story about having dense breast tissue leading to a late-stage cancer. A false negative mammography scan (diagnosed in 2004) concealed a large 2.5 cm suspicious lesion, which was later confirmed to be stage 3c breast cancer. This same cancer had metastasized to 13 lymph nodes. This sparked Dr. Cappello to create the "Are You Dense?" Foundation- an international awareness crusade to better support dense breast diagnostics and initiatives pass legislation to enact laws requiring mammography centers to inform patients about their breast density and the associated cancer risks. Dr. Cappello passed away on Nov 15, 2018, from secondary myelodysplastic syndrome (MDS), a bone marrow cancer that was a complication of her prior aggressive breast cancer treatments. But she ignited a legacy of fighting for improved policies, imaging technologies and advanced research to better address this health crisis that puts the est. 40% of the female population (women with dense breasts) at risk of a false negative reading.PART 1: USE OF ULTRASOUND IN A 2021 RESEARCH STUDY OF BREAST DENSITY
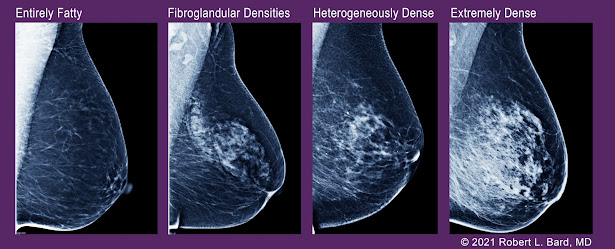
In an ongoing clinical study co-investigated by Dr. Robert Bard (NYC) and Dr. Noelle Cutter (of Molloy College, Long Island, NY), data is collected from a cohort of women undergoing ultrasound density scans. Inspired by Dr. Cappello’s early surveys of specific demographic groups, this 2021 research explores dense breast predominance in the younger population or those with lower body mass index (including dancers and athletes), both are likely candidates to receive false negative readings on a mammogram.In addition, breast density is also associated with breast cancer risk in women between ages 40-65, but there is limited evidence of its association with risk of breast cancer among women 18+. This estimated proportion of breast cancers are attributable to breast cancer risk factors commonly documented in clinical practice and used in breast cancer risk prediction models, including BI-RADS breast density and ultrasounds to confirm mammography readings.
Target Objectives
Endurance athletes are to be defined by those who participated in one or more endurance events (long course) in the year or as well as those who are (younger, low BMI cohort) MD and classification of “dense breasts” was heterogeneous and extremely dense as noted by the BIRADS code; (heterogeneously or extremely dense vs scattered fibroglandular densities). Data is collected as odds ratio (OR’s) and 95% confidence intervals included in research outcomes.Although breast density is a well-established and prevalent breast cancer risk factor, it’s biological connection is not (yet) clearly understood. More research is needed to support the population associated risk proportion in athletic pre-menopausal women. The data gathered from this study reviews a cohort of women undergoing imaging ultrasound scans of pre-menopausal women with dense breasts. Anecdotally, 50 years ago one never saw a 35-year-old with breast cancer. Twenty years ago, it was common to see women in their 20s with cancer. Environmental factors and toxic substance carcinogenic effect may be a byproduct of the research outcome.
Non-invasive Imaging options
1) Diagnostic Ultrasound meets the scanning requirements and is performed in the office setting accurately and rapidly due to the high resolution and low cost of today’s sonographic equipment. Furthermore, advances in the computerization of the imaging, blood flow, and tumor measures of exact volume and vessel density are now less operator dependent- adding ease of use for this or any clinical research requiring the use of ultrasound technology. This provides a reliable and repeatable diagnosis, and a means to follow the individual’s unique pattern of cancer development, progress, and response to treatment.
Recent technological advances also make these procedures available to much broader clinical application, without requiring years of very unique training and clinical experience, for example, with diagnoses of cystic versus solid lesions. Accuracy in assessing breast [1] tumors and metastatic foci has been documented. It must be emphasized that the beginner will find many confusing artifacts and findings should be confirmed with all pertinent imaging modalities.
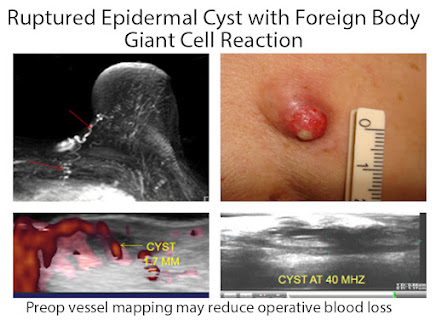
2) 3D Doppler Ultrasound with Dynamic Contrast Enhanced MRI are the gold standards by which cancers are initially diagnosed or confirmed and serially followed after treatment. The percentage of malignant vessels can be quantified and re-evaluated in the identical tumor volume as serial follow ups to the standard treatments using radiation, surgery, hormones, chemotherapy, cryotherapy, watchful waiting and the non-standard regenerative treatments: ablation using focal laser, focal ultrasound, photodynamic, radiofrequency and microwave technologies. Since vessel mapping is possible, embolic treatments may be considered.
3) 3D Sonography can demonstrate the tumor volume and marginal capsule of locally affected lymph nodes more accurately than the MRI since the resolution is 100 microns at 18 MHz. The exam takes about 10 minutes, and the probes are automated meaning that this is less operator dependent than other sonographic procedures. Vessel density index (VI) imaging is performed on the data set at an independent workstation and comparison made with prior exams if available.
4) 3D Power Doppler indices vary according to the tumor stage, the histologic grade, capsular disruption, and lymph node metastases. Histologic grade has been studied with this technology and the following approximation has proven useful in prostate tumor staging. This quantitative measure of neovascularity was initially applied to prostate cancer. [2] While it does not exactly correlate with histologic Gleason grading since this is a current functional measure while the microscopy is purely anatomical and may not represent current aggressive potential. It’s predictive value of aggression could be studied in the context of breast and other cancers [3,4]
Medical imaging can map the arteries, veins and nerves providing preoperative landmarks reducing postoperative bleeding and avoiding nerve damage. Tumors of low aggressive potential may be treated medically and followed by interval scans or locally reduced by radiation or laser ablation. Biopsies of certain abnormalities may be averted or postponed. (FIG 1)

High tumor vessel density correlates with greater aggression. Axillary and mediastinal imaging can document lymphadenopathy. Abdominal scans simultaneously performed may detect ascites and metastases to the liver, periaortic nodes and pelvic organs. Response to neoadjuvant chemotherapy may be assessed MRI, CT, mammography, PET/CT and ultrasound. The new technology of ultrasound elastography, assessing tumor stiffness, predicts response to treatment accurately and may indicate better therapeutic strategies on a timelier basis. [5] Residual cancer burden scoring could provide better treatment options since the treatment response for evaluation of neoadjuvant chemotherapy needs a more comprehensive and authoritative standard than is currently available.
Lymph Node Disease
Lymph node assessment is possible at the same time. Under sonographic guidance, biopsies may be obtained. Sonographic criteria for malignancy are published elsewhere. Image guidance of enlarged node can distinguish between active tumor and necrotic areas diminishing necessity of repeated aspirations for indeterminate findings. (Fig 2) Pathologic assessment of a large postoperative specimen may be facilitated by high frequency scanning to re-localize the suspect region for targeted study that has been removed from its previous anatomic position. [6] Elastography is useful in targeting sub-centimeter foci in large nodal masses
Part 3: IMAGE GUIDED BIOPSY AND TREATMENT
New computer programs use nanotechnology and cybernetic modalities for accurate image guided biopsy and treatment options. Lesions as small as 3 mm have been successfully imaged at frequencies above 14 MHz. Employing 3D sonography with Doppler, the physician manually targets the area of highest tumor neovascularity. This is critical since only part of a mass may be cancerous and missed on non targeted punch biopsies. The marriage with fusion of MRI with ultrasound permits image guided biopsies that spare the adjacent vascular channels. The same technology allows customized ultrasound or MRI guided biopsies to be performed under local anesthesia. Immediate cytologic confirmation of tumor cells permits the withdrawal of the biopsy needle and insertion of a LASER fiber or cryogenic probe immediately treating the proven tumor. MRI thermocoupled sensors prevent overheating of the adjacent nerves and sensitive tissues. Following ablation, the zone of destruction is confirmed with Doppler, contrast ultrasound or DCE-MRI. Inflammatory lesions that are deeply seated may be approached by robotic image guided subdermal injections or targeted biopsies if necessary. This outpatient procedure allows the patient to return to work immediately. RF thermoprobes with temperature auto cutoffs prevent thermal skin damage.[7] Similar user friendly and cost-effective modalities may replace other therapies in the near future. At the 2016 AMERICAN SOCIETY OF LASERS IN MEDICINE meeting in Boston, cutaneous melanoma with in-transit metastases was successively treated by laser technologies [8] MRI Fusion Biopsies with CT and/or ultrasound are routine adding further to the accuracy of image guided biopsies and focal treatment procedures. [9]
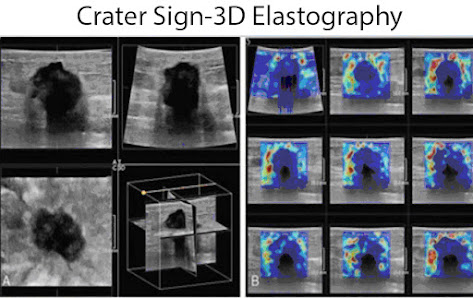
Advances in ultrasound elastography progressed from simple strain imaging to shear wave sonography to 3D coronal shear wave elastography where the plane of the image corresponds to the surgical field as the tumor is dissected in the most superficial plane. The tumor desmoplasia in the coronal plane creates a sawtooth irregular border with a central echo pattern simulating a “donut” and is termed the “crater” sign in this increasingly popular imaging paradigm. Elastography is used worldwide primarily in the diagnostic workup of breast, thyroid and prostate tumors and has reduced the number of biopsies on false positive findings from mammography, b-mode ultrasound and MRI.[10]
Fig. 3 - Mixed solid/necrotic axillary lymph node-vessel density allows targeting of active disease
References
1. Bard R. Vascular imaging of cancer in the dense breast. 60th Journees Francaises de Radiologie 2012, Paris
2. https://www.breastcancer.org/symptoms/understand_bc/statistics
3. Cruwys, Cheryl, and JoAnn Pushkin. “Breast density and impacts on health.” ecancermedicalscience 11 (2017).
4. Nazari, Shayan Shaghayeq, and Pinku Mukherjee. “An overview of mammographic density and its association with breast cancer.” Breast cancer 25.3 (2018): 259-267.
5. Boyd, Norman F., et al. “Mammographic density: a heritable risk factor for breast cancer.” Cancer epidemiology. Humana Press, 2009. 343-360.
6. Burton, Anya, et al. “Mammographic density and ageing: A collaborative pooled analysis of cross-sectional data from 22 countries worldwide.” PLoS medicine 14.6 (2017): e1002335.
7. Azam, Shadi, et al. “Determinants of mammographic density change.” JNCI Cancer Spectrum 3.1 (2019): pkz004.
8. Boyd, Norman F., et al. “Body size, mammographic density, and breast cancer risk.” Cancer Epidemiology and Prevention Biomarkers 15.11 (2006): 2086-2092.
9. Bard R. Image guided cancer treatment. Advances in Medical and Surgical Dermatology, 15th Annual Mt Sinai Winter Symposium New York 2015.
10. Merce L, Alcazar J, Lopez C et al. Clinical usefulness of 3-dimensional sonography and power Doppler angiography for diagnosis of endometrial carcinoma. J Ultrasound Med 2007; 26:1279-1289.
Disclaimer & Copyright Notice: The materials provided on this website/web-based article are copyrighted 2021 and the intellectual property of the publishers/producers (The NY Cancer Resource Alliance/IntermediaWorx inc. and Bard Diagnostic Research & Educational Programs). It is provided publicly strictly for informational purposes within non-commercial use and not for purposes of resale, distribution, public display or performance. Unless otherwise indicated on this web based page, sharing, re-posting, re-publishing of this work is strictly prohibited without due permission from the publishers. Also, certain content may be licensed from third-parties. The licenses for some of this Content may contain additional terms. When such Content licenses contain additional terms, we will make these terms available to you on those pages (which his incorporated herein by reference).The publishers/producers of this site and its contents such as videos, graphics, text, and other materials published are not intended to be a substitute for professional medical advice, diagnosis, or treatment. For any questions you may have regarding a medical condition, please always seek the advice of your physician or a qualified health provider. Do not postpone or disregard any professional medical advice over something you may have seen or read on this website. If you think you may have a medical emergency, call your doctor or 9-1-1 immediately. This website does not support, endorse or recommend any specific products, tests, physicians, procedures, treatment opinions or other information that may be mentioned on this site. Referencing any content or information seen or published in this website or shared by other visitors of this website is solely at your own risk. The publishers/producers of this Internet web site reserves the right, at its sole discretion, to modify, disable access to, or discontinue, temporarily or permanently, all or any part of this Internet web site or any information contained thereon without liability or notice to you.